Kidney stones are formation of hardened minerals in the kidneys or urinary system.In most cases,it is because of decrease in urine volume or increase in the minerals that form the stones in urine.
Kidney stones in some cases can actually result in a “dead” kidney or kidney failure. The good news though is that this doesn’t happen very often and it often takes a long time to occur, providing the opportunity for treatment to occur before permanent damage occurs.
Kidney stones can cause kidney damage in two primary ways.
An untreated obstructing stone that causes persistent severe blockage instead of successfully passing can eventually cause atrophy in a kidney, resulting in a dilated, thinned out kidney with minimal function.
Thankfully, because most stones are associated with significant amounts of pain, most patients will seek treatment long before permanent damage can occur.
However, in cases where patients have “silent” stones that cause little or no pain, long term obstruction can occasionally lead to kidney damage. With no symptoms to warn them, these patients often go months to years before a stone is diagnosed.
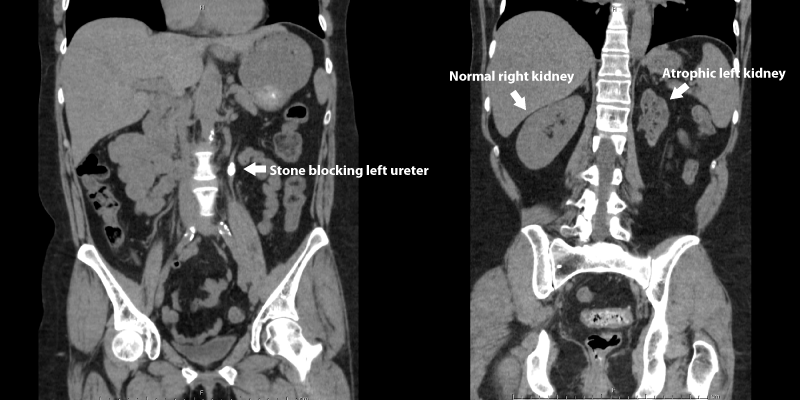
The CT scan below demonstrates a left kidney which has been damaged by a large obstructing left ureteral stone. For comparison, note the normal size right kidney. The patient did not have any symptoms of pain and the stone was found after the CT scan was obtained for the finding of blood in the urine.
2) Infection related stones, usually composed of struvite and sometimes presenting as a complete “staghorn” can lead to ongoing chronic urinary tract infections that cause damage slowly through inflammation and scarring of the kidney tissue.
One reason why kidney stones don’t often cause chronic kidney disease or failure more often is because in most cases, kidney stones will cause damage to only one kidney. Patients whose other kidney is healthy will usually not develop kidney failure.
Exceptions to this can occur in cases of kidney stones affecting both kidneys, large infection stones occurring in both kidneys, certain congenital causes of kidney stones, and in patients with only one kidney
The most common symptom is severe, fluctuating pain that starts in the area where the kidneys are located, in the lower
back or side under the ribs. Pain tends to move with the stone. If the stone stops, the pain may stop. Other symptoms
include:
- Bloody or cloudy urine that smells bad
- Nausea and/or vomiting
- Fever and/or chills
- Burning, painful sensation when urinating
If you have any of these symptoms, please call your doctor. Taking care of kidney stones early can prevent serious
complications, such as CKD or, in extreme cases,RENAL FAILURE that would require DIALYSIS or a KIDNEY
TRANSPLANT to replace the function of the kidneys.
Treatment for kidney stones
Determining the type of kidney stone you have is usually done by evaluating a 24-hour collection of urine, or by
examining a stone after it has been passed. There are several methods of renal stone removal; many don’t require
surgery. You may even be able to pass a stone by drinking lots of water.
Some of the treatments for kidney stones that are too large to pass, or are causing damage, include:
1.Shock waves that are sent directly to the kidney stone. Extracorporeal shock wave lithotripsy (ESWL) or sound waves is not an invasive treatment, so it doesn’t usually require surgery or a hospital stay.
2.Nephrolithotomy, or percutaneous (meaning “through the skin”) nephrolithotomy, is when the doctor makes a small incision in your back and removes the kidney stone using a nephroscope and lithotripter.
3.Ureteroscopic kidney stone removal is a procedure that uses a scope passed through the bladder to remove a stone that is stuck in the ureter after fragmenting with a holmium laser.
How can I avoid developing kidney damage from my stones?
The good news is that for the vast majority of kidney stone patients, significant kidney damage is unlikely. To be on the safe side, there are a few steps you can take.
- If you develop a stone episode but do not pass a stone or undergo treatment within a few months, you may want to consider getting followup imaging with your doctor to insure that the stone has actually passed and is not causing persistent obstruction. This is more of a concern for larger stones (greater than 6mm or so).
- Patients with large infection related stones (struvite) are at increased risk for kidney damage from their stones. They should be sure to have their stones treated and need followup to insure infections and stones do not return.
- Work with your doctor to prevent future stones. A Stone prevention plan may include testing for the reason why you are forming stones, diet changes, or in certain cases, medications.










































.jpg)